Bu içerik, genç yaşında endometriozis ve adenomyozis nedeniyle yaşadığı zorlukları anlatan Emily Griffiths’in hikayesini içeriyor. Emily, hastalıklarının neden olduğu şiddetli ağrılar ve evden dışarı çıkamama gibi belirtilerle mücadele ediyor. Histereskopi ameliyatı olmayı düşünen Emily, ancak doktorların yaşına ve çocuk sahibi olmamasına takılarak konuyu tartışmaya yanaşmadıklarını belirtiyor. Hikayesi, kadınların kendi vücutları üzerinde özgür bir seçim yapma hakkının kısıtlandığı, sağlık hizmetlerindeki eksikliklerin ve uzun bekleme sürelerinin neden olduğu zorlukları vurguluyor. Ayrıca, hikaye, Emily’nin kronik hastalıklar ve engellilik konusunda farkındalık yaratma çalışmaları nedeniyle Kraliçe ve Prenses tarafından tanındığını da belirtiyor. Mevcut sağlık politikalarının ve tedavi seçeneklerinin eleştirildiği bu içerik, genç ve endişeli kadınların yaşadığı zorlukları gözler önüne seriyor.
[ad 1]
Kaynak: www.bbc.com

 Emily Griffiths
Emily GriffithsEmily Griffiths wants to have an operation to remove her womb, known as a hysterectomy.
At 26, with no children, she knows it is a big step. But endometriosis and adenomyosis have left her housebound, in debilitating pain, and unable to see a future as a mum.
Right now, she simply dreams of being able to go for a walk unaided. But she says she has been unable to find a clinician who will discuss the procedure because of her age.
“Doctors are too busy planning ahead for the child I might want in the future and can’t see where I am right now,” said Emily, from Carmarthenshire.
Emily’s symptoms started when she was 12, with periods so painful and heavy that she missed school and became anaemic.
She said GPs told her the pain was normal.
“They would say it was all in my head and I was just trying to be off school,” she said.
Emily was diagnosed with endometriosis aged 21, after collapsing with sepsis.
She was referred to a specialist centre in Cardiff, but said the wait was so long that her family self-funded private surgery.
Emily, who has been unable to see an NHS specialist, said she had lost count of the private clinicians she had seen and felt there was “zero support” from the health service.

 Emily Griffiths
Emily GriffithsA hysterectomy would leave Emily infertile and prompt the menopause, which in turn could increase her risk of osteoporosis, heart disease and dementia.
Yet for the past three years she has been given a monthly injection to chemically induce menopause, pausing her periods in an effort to alleviate her symptoms.
Scans show that has caused her bone density to deteriorate.
“A hysterectomy isn’t a cure for endometriosis, but it is for adenomyosis,” she said, adding she was 23 when she received that additional diagnosis.
“Even though it’s a big step, I could have the possibility of maybe going for a little walk when I’m really struggling… but at the moment I’m stuck in a very dark place.”
What is a hysterectomy?
A hysterectomy is a major operation with a long recovery time which is only considered following less invasive treatments.
It is carried out to treat health problems affecting the female reproductive system.
A total hysterectomy is the surgical removal of the womb and cervix.
In some cases the fallopian tubes, ovaries, lymph glands, and part of the vagina, can also be removed.
What are endometriosis and adenomyosis?
Adenomyosis is a condition where the lining of the womb starts growing into the muscle in the wall of the womb.
It can cause painful periods and heavy bleeding, as well as pelvic pain, bloating and pain during sex.
Endometriosis is where cells similar to those in the lining of the womb grow in other parts of the body.
Symptoms happen when those patches break down and bleed but cannot leave your body.

 Emily Griffiths
Emily GriffithsEndometriosis is currently widespread across both of Emily’s ovaries as well as her uterus, bladder and part of her bowel.
Her menopausal symptoms have also been severe, but hormone replacement therapy (HRT) makes her endometriosis worse.
Because of the complexities of her case, Emily would need an endometriosis specialist to carry out the hysterectomy as it would also involve excision of the endometriosis.
A hysterectomy is listed as one of a number of treatment options by NICE for endometriosis and adenomyosis.
Endometriosis UK said a hysterectomy could not guarantee total loss of pain and symptoms, but “it’s important to remember that the final choice is yours – it is your body”.
Emily said that sentiment was at odds with her own experience.
‘Told I’m too young’
“I don’t really think that women do have the freedom to make a choice over their own bodies,” she said.
“I’ve been told that if I settle down ‘you may want to have a child with your husband’ – it’s just planning ahead and not seeing where I am right now.
“Basically fertility has been put way above any of my illnesses and what I’m going through.”
Emily said she had been advised to stay in a chemically-induced menopause, try the contraceptive pill or anti-depressants, along with “running, pilates or yoga”.
“I can’t walk without support, so to tell me about pilates or running is not the nicest comment,” she said.

 Emily Griffiths
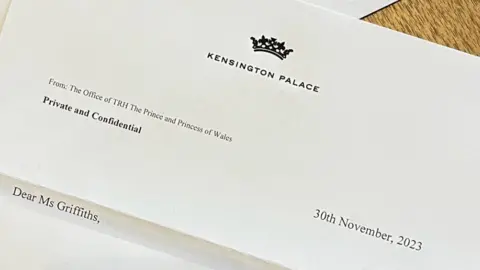
Emily GriffithsEmily’s work to raise awareness of the issues she faces has earned her recognition from the King and the Princess of Wales.
“I’ve had some really amazing opportunities… and that’s what’s keeping me holding on to some sort of hope,” she said.
There are currently two accredited NHS endometriosis centres in Wales, in Swansea and Cardiff.
The centre in Swansea does not currently accept patients from outside the health board area, while Cardiff said it considers outside referrals “where appropriate”.
Every health board has endometriosis nurses to support patients, but Emily, who lives in the Hywel Dda health board region, said lengthy waits meant she had little option but to seek private care.
“There’s been two privately funded surgeries so far, with possibly another one coming,” said Emily.
Follow-up care and advice also comes at a cost.
“No one on the NHS will monitor me currently, so it does become a never ending cycle of funding and finding the right person,” she said.
“If you have a question, maybe a certain medication they’ve prescribed isn’t agreeing with me, it always comes at a cost, you can’t simply ring them and find out.
“I understand that’s the route you take when you have private care, but if the NHS aren’t there to help either, then there’s no choice.”
Sioned Williams, Plaid Cymru’s spokesperson for social justice and equalities, was made aware of Emily’s case after she raised it with her local Member of the Senedd (MS).
“The Welsh government has been too slow in delivering their women’s health plan,” Ms Williams said.
“People with endometriosis such as Emily just want to be heard and believed and this should not be too much to ask.”
Sam Rowlands, the Welsh Conservative health spokesperson said: “The Welsh Conservatives would immediately scrap the restrictive NHS guidance that locks patients in their local area, blocking cross-community and cross-border working, to make use of extra capacity to reduce excessive NHS waits in the short term and look to enact a substantial workforce plan to tackle the more deep-seated issues in the longer term.”
A Welsh government spokesperson said it had made women’s health “a key priority” and would publish a 10-year women’s health plan in December.
“The Women’s Health Network, led by the first ever clinical lead for women’s health in Wales, has been established to deliver improvements including in endometriosis care, treatment and support,” they said.
“Health boards are responsible for delivering services and we have funded dedicated endometriosis nurses within each health board.”







Yorumlar kapalı.